Every one of us “doctors” when he/she first enter the hospital as an junior resident, intern or medical student, face difficulty in writing a proper progress note at the first time. Sometimes, our progress note makes our consultant or senior resident upset, and we got a lot of bad comments on it. Sometime you can’t find someone to help you how to write it.
In this paper, I will try to give you some valuable points in writing the progress note and samples of it, from my experience and what I learned from previous colleagues. First, I will start by discussing the importance of progress note. Second, how to write it and at the end, I will give samples for it.
Importance of progress note:
- To give daily updates on your patients: illnesses, diagnosis, and treatment.
- A way of communication to colleagues and the healthcare team collaborating in treating your patient.
Remember that the progress note is not an assignment to show your medical knowledge to get a good grade.
Writing the PROGRESS NOTE:
- There are basics in writing any medical documentation:
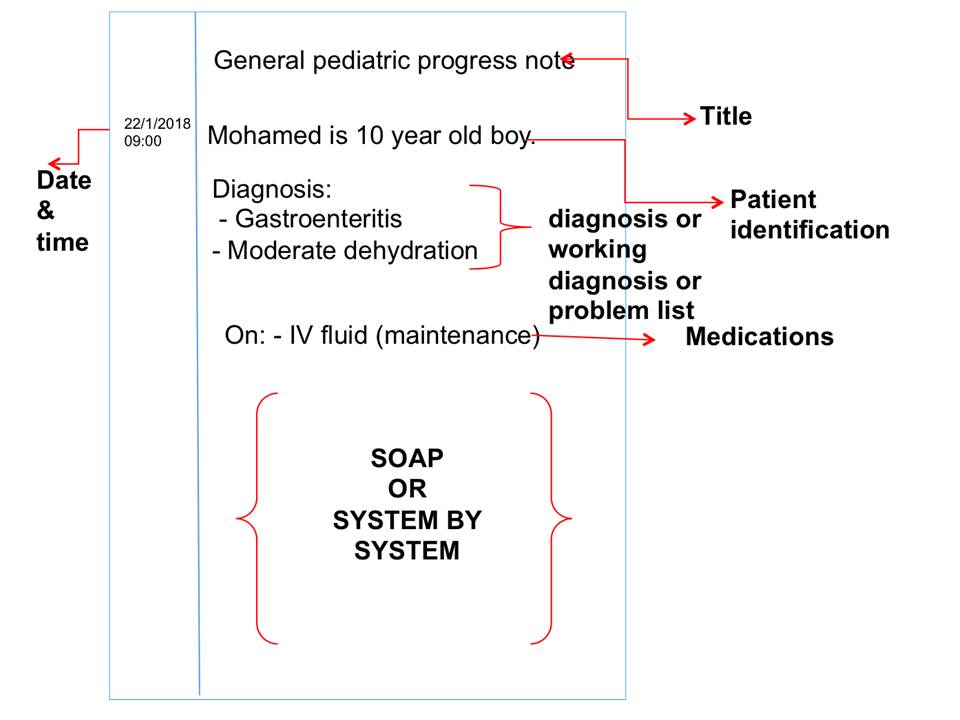
- Date and time all notes.
- Include a brief title for example “ General pediatric progress note/physical therapy progress note.”
- Avoid abbreviations.
- Don’t cut and paste from previous notes without editing and updating.
- Unethical and Unprofessional to use another doctor’s observations or assessments.
- When you sign the notes, be sure to print your name legibly and include your pager number
- Progress note:
- Patient identification (name, age, file number)
- Diagnosis/ working diagnosis/ problem list
- Medication
- You will use one of two styles in writing the note “SOAP” or “System by system”.
SOAP format:
| Part | Discussion |
| S (subjective) |
|
| O (objective) | This is the focused on physical examination & investigation
|
| A(assessment) |
|
| P (plan) |
|
** in case if you have multiple problems or working diagnosis in the patient what you need to write in the assessment & plan A/P?
In this condition:
- You have to prioritize the diagnoses. ” the most acute problems addressed first”
- Use “bullet” and write each key working diagnoses and how the patient is responding.
For example:
A/P: Reem is 50 year old woman with:
- Left lower lobe pneumonia likely pneumococcus with improved O2 sats on day 2 levofloxacin.
- Uncontrolled type 2 DM with improved glucose control, and resolving hypovolemic hyponatremia.
**Hint: Don’t keep repeating the same amount of detailed explanations in the A/P that you gave on day 1. This will leads to the 2-3 page progress note that no one like to write or read. No need to discuss resolved issues every day in progress note.
System by system format:
You can divide your progress note to a system in each one it will include subjective/ objective/ medication.
- Respiratory system
- Cardiovascular system (CVS)
- Gastroenterology system (GIT)
- Infectious (ID)
- OTHERS
**there will be example later on.
A good progress note:
- Focused
- Targeted
- Well organized
- Specific
- Updated daily
- Has a plan
- User friendly!
Good Luck
How to write proper Medical progress note?
By Dr.Dana Aljindan
“Pediatrician”